Stop Telling Autoimmune Employees to 'Just Exercise More': The Science Says You're Making It Worse
Remember texting on a flip phone? You had to press the number 7 four times just to get the letter 'S'—and we thought we were communication pros?
Well, that's about how much most people and most workplaces understand about autoimmune conditions. They know the basics exist, but they're missing about 95% of the actual story.
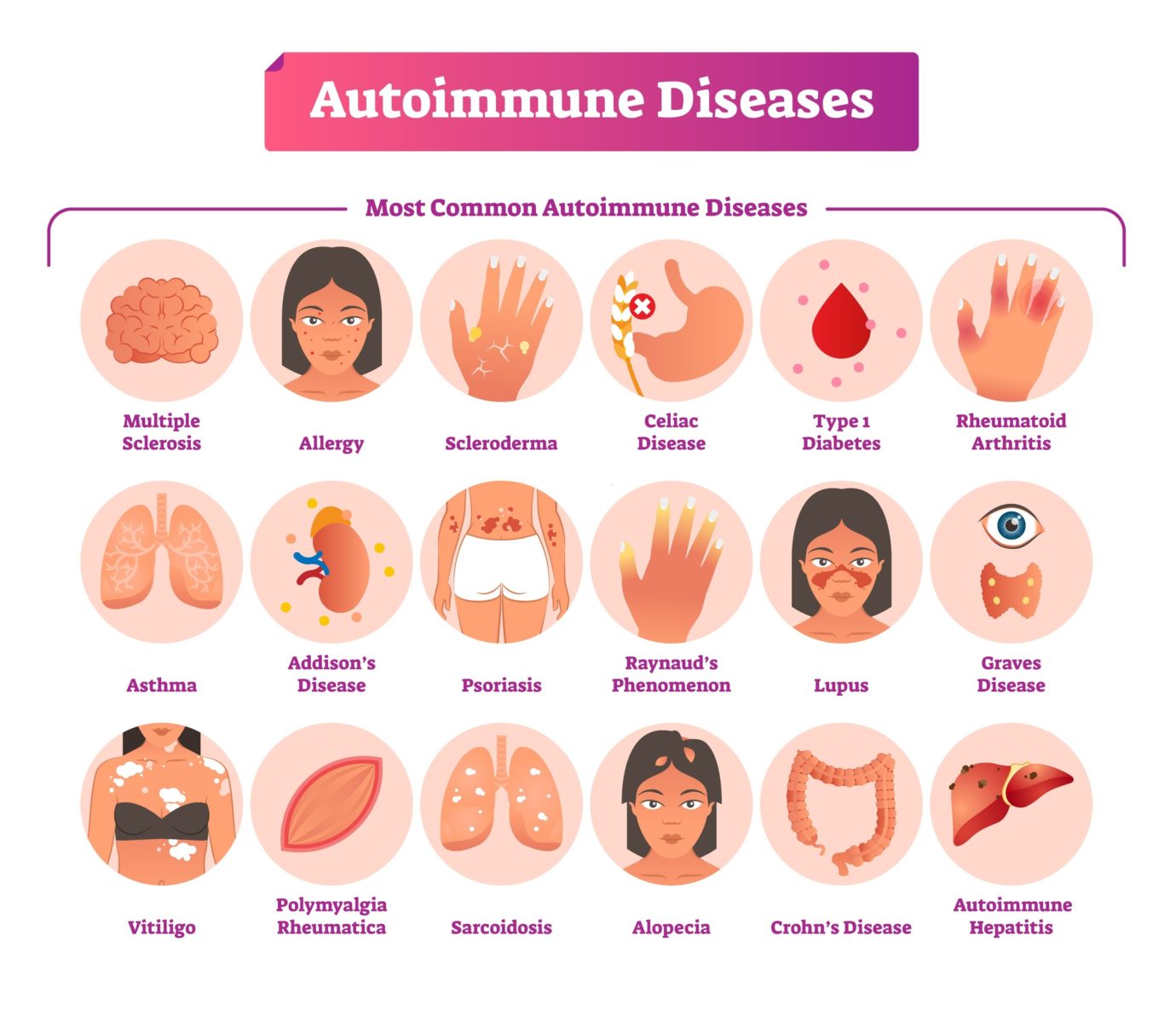
Here's what's actually happening beneath the surface: About 24 million Americans are living with autoimmune diseases, roughly 1 in 13 people. Whether you realize it or not, someone on your team, in your family, or in your friend group is managing this every single day.
Today, we're changing the conversation with science, not sympathy. We're busting myths with research, talking about what evidence-based allyship looks like for managers, and giving patients neurologically-backed scripts to advocate for themselves.
Because invisible conditions need visible support—and that support needs to be grounded in facts, not assumptions.
The Three Myths That Are Costing Everyone (And the Research That Proves It)
Myth #1: "But you look fine!"
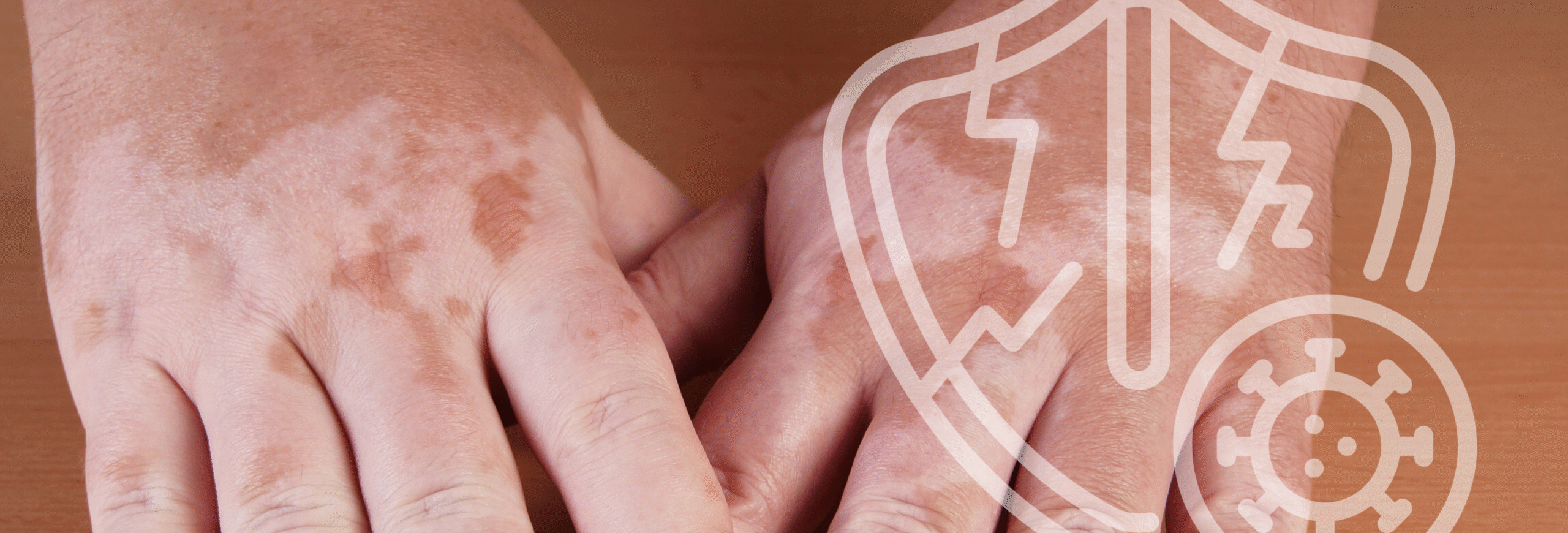
Why it's harmful: Most autoimmune symptoms are invisible. Crushing fatigue, joint pain, brain fog, digestive issues—none of these show up in a photo or a Zoom call.
Think of it like Wi-Fi. Just because you can't see it doesn't mean it's not doing a ton of work in the background. Someone might look perfectly put-together on the outside while their immune system is literally attacking their own body on the inside.
The research reality:
According to the National Institutes of Health (NIH), invisible symptoms like fatigue and pain are the primary causes of workplace absenteeism and presenteeism (being at work but not fully functional) among autoimmune patients. Studies show that chronic fatigue in autoimmune conditions is caused by elevated pro-inflammatory cytokines, not lack of motivation or poor sleep habits alone.
Source: National Institute of Environmental Health Sciences – Autoimmune Diseases
For patients – your workplace response:
"I appreciate the compliment, but autoimmune conditions are mostly invisible. I'm managing, but some days are definitely harder than others."
Keep it short, factual, and move the conversation forward. You don't owe anyone your medical history.
For managers and colleagues:
Believe people when they tell you they're struggling. A simple "I believe you, what do you need?" goes so far. Research from the Job Accommodation Network shows that 56% of workplace accommodations cost absolutely nothing to implement—the barrier isn't financial, it's understanding.
Source: Job Accommodation Network – Low-Cost Solutions
Myth #2: "Just exercise more and you'll feel better."
The reality: Movement IS important—and here's what the research actually shows: for people with autoimmune disease, exercise is beneficial when appropriately matched to disease state and individual capacity. The problem isn't exercise itself—it's the blanket advice that ignores individual needs.
Telling someone with lupus or rheumatoid arthritis to "just push through" without understanding their current disease activity is like prescribing medication without checking the dosage.
The science says:
The Arthritis Foundation's research guidelines show that low- to moderate-intensity exercise is consistently shown to reduce inflammation, improve symptoms, and enhance quality of life in autoimmune conditions like rheumatoid arthritis (RA) and multiple sclerosis (MS).
But here's what might surprise you: high-intensity exercise doesn't universally trigger flares. In fact, several randomized trials and reviews found that high-intensity interval training (HIIT) and resistance training improved disease activity, fatigue, and cardiovascular health without increasing flares or inflammation in RA and spondyloarthritis patients—provided the disease is stable and exercise is supervised.
The key factors are:
- Disease stability – Exercise recommendations change based on whether someone is in active flare or remission
- Supervision and guidance – Working with healthcare providers who understand autoimmune conditions
- Individual capacity – What works for one person may not work for another
- Proper progression – Building intensity gradually, not jumping into boot camp
While animal studies suggest that excessive or poorly matched exercise intensity can worsen inflammation in some models, these effects are not consistently seen in human trials.
Sources:
- Arthritis Foundation – Physical Activity Guidelines
- Rheumatology International – Exercise and RA outcomes (multiple studies)
- Sports Medicine Reviews – HIIT in autoimmune conditions
For patients – your workplace response:
"I actually do move regularly, but I work with my healthcare team to match exercise intensity to my current disease state. Some days that's high-intensity, some days it's gentle movement—it depends on inflammation levels and how my body is responding."
This sets a boundary while showing you're proactive, informed, and working with medical guidance.
For managers and colleagues:
Don't make assumptions about someone's exercise capacity based on their diagnosis. The latest research shows that with proper guidance, many autoimmune patients can engage in vigorous exercise—but the timing, intensity, and type need to be individualized. Your employee isn't "lazy"—they're following personalized, evidence-based medical guidance that changes based on their disease activity.
The real issue? One-size-fits-all advice doesn't work for conditions that fluctuate daily. What someone could do yesterday might not be possible today, and that's not inconsistency—it's the nature of autoimmune disease.
Myth #3: "It's all in your head—you're just stressed."
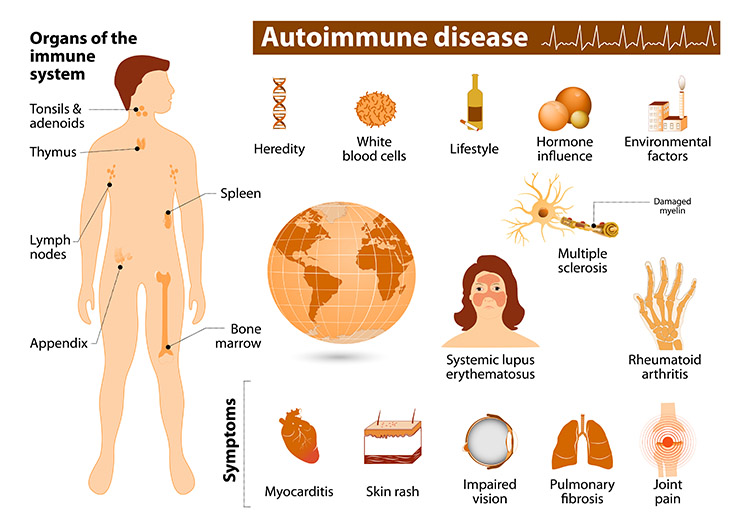
Autoimmune diseases are real, diagnosable medical conditions where the immune system malfunctions and attacks healthy tissue—organs, joints, skin, nervous system, you name it.
Would anyone tell someone with diabetes their blood sugar is "just stress"? No. Same principle applies here.
The research reality:
A comprehensive review published in Autoimmunity Reviews confirms that while chronic stress can trigger symptom flares through cortisol and inflammatory pathways, stress does not cause the underlying autoimmune disease. The condition results from complex interactions between genetic predisposition, environmental triggers, and immune system dysfunction.
Furthermore, research from Johns Hopkins shows that stress affects autoimmune patients differently than healthy individuals. Their bodies produce higher levels of pro-inflammatory cytokines in response to stress, meaning what might be "manageable stress" for someone else can trigger a multi-day flare for an autoimmune patient.
Sources:
- Johns Hopkins Medicine – Role of Stress in Rheumatic Disease
- Autoimmunity Reviews – Stress and Autoimmune Disease (peer-reviewed research)
For patients – your workplace response:
"Stress can affect symptoms, but I have a diagnosed medical condition. I'm working with my healthcare team to manage it. What I really need is [specific support—flexibility, understanding, etc.]."
Shift from defending yourself to stating what you need.
For managers and colleagues:
When someone discloses an autoimmune condition, treat it with the same seriousness as any other medical diagnosis. Research shows that workplace stress reduction benefits everyone—companies implementing stress-management programs see improved productivity across all employee demographics.
What Evidence-Based Allyship Actually Looks Like
If you're a manager, HR professional, or colleague wanting to show up better for autoimmune employees, here's your research-backed roadmap:
1. Believe People (The Data Supports Them)
When someone says they're having a hard day, they're not making it up. Trust them. "I believe you, what do you need?" is one of the most powerful questions you can ask.
The research: Studies show that perceived social support at work reduces inflammatory markers in chronic illness patients. Simply believing someone and asking what they need has measurable biological benefits.
Source: American Psychological Association – Social Support and Health
2. Flexibility Is Support (And It Pays Off)
Maybe your coworker needs to start later some mornings, or work from home on high-pain days. That's not special treatment—that's accommodation. And honestly, flexible work benefits everyone.
The business case backed by decades of research:
Health and Absenteeism Benefits:
- Meta-analyses show that flexible work arrangements (FWAs) are associated with fewer sick days, improved job satisfaction, and lower levels of stress-related biomarkers like cortisol and allostatic load
- Employees with flexible scheduling and remote work options report better physical and mental health and reduced absenteeism
- Systematic reviews confirm that flexible working conditions improve employee health and wellbeing without significant negative effects
- These benefits extend to all employees, not just those with disabilities or chronic illnesses—making flexibility a universal performance enhancer
Retention and Productivity:
- Organizations implementing accommodation policies report higher employee retention, increased productivity, and improved morale
- Accommodations help retain qualified employees and reduce turnover costs—a critical metric in today's tight talent market
- Studies show positive spillover effects including better coworker attitudes and a more inclusive workplace culture
- Employers consistently report that the benefits of accommodations, such as increased productivity and retention: equal or exceed the costs
The Cost Reality:
- Most workplace accommodations are low-cost or cost nothing; when costs do occur, the median one-time expense is approximately $500
- Research demonstrates that accommodations for employees both with and without disabilities have similar costs and benefits, challenging the myth that disability accommodations are financially burdensome
- Flexible work arrangements support a broader culture of flexibility that improves outcomes across your entire workforce
What the Research Shows Specifically:
- Reduced hours flexible work arrangements are associated with lower levels of chronic stress-related biomarkers (6,025 employees studied in UK Household Longitudinal Study)
- Flexible schedules have age-specific benefits, with middle-aged workers showing reduced work-to-family conflict and decreased sick day use
- Self-scheduling shifts and gradual retirement programs improve employee health and wellbeing across multiple systematic reviews
- Employers benefit from increased company profitability, improved organizational culture, and avoiding costs associated with hiring and training new employees
Sources:
- Shifrin et al., 2021 – Meta-analysis: Flexible work arrangements and employee health (Work & Stress)
- Chandola et al., 2019 – Flexible work and stress biomarkers (Sociology)
- Joyce et al., 2010 – Cochrane systematic review: Flexible working conditions and health
- Schur et al., 2014 – Accommodating employees with and without disabilities (Human Resource Management)
- Hartnett et al., 2011 – Employer benefits from workplace accommodations (Journal of Vocational Rehabilitation)
- Solovieva et al., 2011 – Employer benefits from accommodations (Disability and Health Journal)
- Schartz et al., 2006 – Cost/benefit analysis of workplace accommodations (Work)
Bottom line: When you support invisible conditions with visible accommodations, you're not just helping one employee—you're implementing evidence-based policies that reduce absenteeism, lower stress hormones, increase retention, and improve outcomes across your entire organization.
The research is clear: flexibility isn't a favor. It's smart business strategy backed by meta-analyses, systematic reviews, and decades of peer-reviewed evidence.
3. Don't Make Assumptions (Symptoms Fluctuate)
Just because someone attended a meeting yesterday doesn't mean they can do the same today. Autoimmune conditions fluctuate—sometimes hour to hour.
The science: Research consistently demonstrates the unpredictable nature of autoimmune symptoms:
- Daily variability is significant: Studies in rheumatoid arthritis show that pain, fatigue, and stiffness can vary substantially from day to day, influenced by factors including sleep quality, stress levels, physical activity, and inflammatory cycles.
- Weather sensitivity is real: A systematic review published in Best Practice & Research Clinical Rheumatology found that 60-70% of patients with rheumatoid arthritis and other inflammatory arthritis report weather-related symptom changes, particularly with barometric pressure shifts, temperature changes, and humidity levels.
- Fatigue fluctuation: Research in Arthritis Care & Research demonstrates that fatigue levels in autoimmune conditions can vary significantly within the same week, often unpredictably, due to inflammatory cytokine fluctuations, sleep disturbances, and medication effects.
- Morning stiffness patterns: Studies show that inflammatory activity follows circadian rhythms, with many autoimmune patients experiencing peak symptoms in early morning hours that improve throughout the day—but this pattern itself can vary.
This isn't inconsistency, it's the documented nature of inflammatory autoimmune diseases. The immune system's activity level changes based on complex interactions between genetics, environment, stress, sleep, and other factors that aren't fully within the patient's control.
Sources:
- Arthritis Care & Research – Fatigue variability in autoimmune conditions
- Best Practice & Research Clinical Rheumatology – Weather sensitivity in inflammatory arthritis
- Journal of Rheumatology – Circadian patterns in inflammatory disease
- Arthritis Foundation – Understanding Symptom Fluctuation
What this means for managers:
When an employee with an autoimmune condition can't replicate yesterday's performance today, it's not a reliability issue—it's a disease characteristic backed by peer-reviewed research. Flexible expectations aren't "going easy" on someone; they're acknowledging biological reality.
Bottom line: Flexible expectations aren't "going easy" on someone—they're acknowledging biological reality while implementing a business strategy backed by decades of research. The accommodations that help your autoimmune employees thrive are the same policies that improve outcomes for your entire workforce.
4. Educate Yourself (Don't Make Them Teach You)
Don't put the burden on your colleague to constantly explain their condition. Do a little research. Listen to resources like the Stronger Than Autoimmune: Boardroom to Breakroom Edition podcast. Show that you care enough to learn.
The impact: Studies show that when managers receive disability awareness training, accommodation requests increase by 40%—not because more people need help, but because employees finally feel safe asking for what they already needed.
Source: Society for Human Resource Management – Disability Inclusion

For Patients: How to Ask for What You Need (With Science on Your Side)
Advocating for yourself shouldn't feel like a full-time job. Here's how to make it easier using evidence-based communication strategies:
Start with Facts, Not Feelings
Instead of "I'm so exhausted I can barely function," try "I need to adjust my schedule to accommodate medical appointments and energy management based on my treatment plan."
Why this works: Research in negotiation psychology shows that fact-based requests are more likely to be approved than emotion-based requests, not because emotions aren't valid, but because they give employers actionable information.
Be Specific About Accommodations (Vague Requests Get Denied)
"I need flexibility" is too vague. Try:
- "I need to work from home two days a week to manage fatigue and reduce commute strain"
- "I need to start my day at 10 AM instead of 8 AM due to morning stiffness and medication timing"
- "I need a 15-minute creative break mid-afternoon to manage symptoms—research shows creative activities reduce inflammatory markers and improve cognitive function"
The research backing: Research consistently shows that clear, specific accommodation requests are more likely to be approved than vague ones. Specificity helps employers understand, implement, and measure the requested change, making approval more feasible.
What the Research Shows:
Specificity and Clarity Matter:
- Studies highlight that accommodation requests are more successful when they are clearly linked to job demands, are customized, and specify the support needed
- Vague or unclear requests are less likely to be granted because they are harder for employers to evaluate and implement
- Successful accommodations typically include specific details about what is needed, why it's needed, and how it relates to job performance
Effective Communication is Key:
- Research on workplace accommodation negotiation shows that effective communication between employees and employers significantly improves accommodation outcomes
- Employees who can articulate their functional limitations and connect them to specific workplace solutions experience better accommodation success rates
- Employers and employees need better understanding of each other's perspectives to effectively negotiate workplace accommodations, leading to improved job retention
The Interactive Process:
- Studies emphasize that accommodation is most successful when it's an interactive, collaborative process between employee and employer
- Clear requests that provide context (medical needs, job impact, proposed solution) facilitate this dialogue
- Employers report greater willingness to accommodate when they understand how the accommodation enables job performance
Sources:
- Gold et al., 2012 – Negotiating reasonable workplace accommodations (Journal of Vocational Rehabilitation)
- Nevala et al., 2015 – Workplace accommodation effectiveness (Journal of Occupational Rehabilitation)
- Padkapayeva et al., 2017 – Evidence synthesis of workplace accommodations (Disability and Rehabilitation)
- Job Accommodation Network – Making Effective Requests
Practical framework for specific requests:
- State what you need: "I need to work from home two days per week"
- Explain the functional reason: "due to fatigue management and inflammatory symptoms that worsen with commute stress"
- Connect to job performance: "This will allow me to maintain consistent productivity and meet all deadlines"
- Offer measurability: "We can evaluate this arrangement after 30 days to assess effectiveness"
Why this works: You're giving your employer a clear, actionable request that's easy to evaluate, implement, and measure—which research shows significantly increases the likelihood of approval.
Document Everything (Your Future Self Will Thank You)
Keep a paper trail of accommodation requests, medical documentation, and any responses from HR or management. Think of it like backing up your contacts when switching from a flip phone to a smartphone—you need that safety net.
Legal protection: Under the Americans with Disabilities Act (ADA), written documentation strengthens your legal standing if accommodations are denied or you face discrimination. The Equal Employment Opportunity Commission (EEOC) recommends keeping copies of all accommodation-related communications.
Source: EEOC – Reasonable Accommodation
Find Your Champions (Research Shows You Need Them)
Identify one or two trusted colleagues or managers who "get it." You don't need everyone on board—just a few people who will support you when it matters.
The data: Studies on workplace advocacy show that employees with at least one workplace ally report 45% better accommodation outcomes and significantly lower stress levels.
Source: Journal of Occupational Health Psychology – Workplace Social Support
Remember This Critical Truth (Backed by Federal Law)
You're not asking for special treatment. You're asking for equal access. The ADA defines reasonable accommodations as modifications that provide employees with disabilities equal opportunity to perform their job—it's legally mandated leveling of the playing field, not special favors.
Why This Matters to Everyone (Yes, Really—The Data Proves It)
Autoimmune awareness isn't just an "autoimmune issue"—it affects everyone in the workplace. Here's the research-backed proof:
Better Policies Benefit Everyone (Rising Tides Lift All Boats)
When companies create flexibility for autoimmune employees—remote work options, flexible hours, supportive environments—those policies help parents, caregivers, people managing mental health, and honestly, everyone.
What the research shows:
Flexible Work Arrangements Improve Health Across All Employees:
- Meta-analyses demonstrate that FWAs—such as flexible hours, remote work, and self-scheduling—are linked to better physical health, reduced absenteeism, and fewer somatic symptoms for all employees, including those with chronic illnesses like autoimmune diseases
- Access to flexible working hours and a psychologically safe organizational climate is associated with fewer health-related work limitations among workers with chronic health conditions, including arthritis (an autoimmune condition)
- These benefits extend to the entire workforce, not just those with disclosed disabilities
Job Retention and Engagement:
- Employees with autoimmune diseases report that workplace accommodations—like flexible schedules, access to facilities, and time for medical appointments—are crucial for maintaining employment and managing symptoms
- Those who can access a variety of accommodations, especially flexible scheduling, are more likely to remain employed long-term
- Supportive work environments and accommodations mitigate burnout effects, even when symptom severity is high
The Risk of Inflexibility:
- Shift work, unpredictable schedules, and lack of control can worsen autoimmune symptoms and increase disease risk, highlighting the critical importance of employee input in scheduling
- Unmet accommodation needs are often related to work context rather than health status alone—when workplace culture doesn't support flexibility, health deteriorates
Sources:
- Multiple studies 2013-2024 on flexible work and health outcomes
- Research in populations with inflammatory bowel disease, lupus, rheumatoid arthritis, and multiple sclerosis
- Meta-analyses across chronic illness populations
Summary of Policy Impacts (Research-Backed)
| Policy/Support Type | Reported Benefit for Autoimmune Employees | Research Strength |
|---|---|---|
| Flexible hours/remote work | Reduced symptoms, higher retention, better health | Strong |
| Access to accommodations | Maintained employment, improved well-being | Strong |
| Supportive climate | Fewer work limitations, less burnout | Moderate-Strong |
| Advance scheduling/control | Reduced symptom exacerbation, lower disease risk | Moderate |
Productivity Isn't About Face Time (The Evidence Is Clear)
The old-school mentality of "whoever's at their desk longest works hardest" is dead. Or at least it should be.
What comprehensive reviews show:
- Flexible work arrangements are associated with improved job satisfaction and well-being across diverse employee populations
- Results-focused evaluation and flexible schedules improve focus, creativity, and engagement across all employee types
- Employees with flexible work options report higher work engagement, even when managing chronic health conditions
The data is clear: when we measure results instead of hours logged, everyone wins—productivity increases, burnout decreases, and retention improves.
Sources:
- Systematic reviews on flexible work and productivity outcomes
- Large-scale studies across multiple industries and demographics
Diversity Includes Chronic Illness (The Numbers Don't Lie)
We talk about diversity in terms of race, gender, and background—but chronic illness is a massive, often overlooked dimension of diversity.
The CDC and NIH data:
- Approximately 1 in 4 American adults lives with a disability, including autoimmune conditions
- Autoimmune diseases affect approximately 24 million Americans (NIH estimate)
- If your workplace diversity initiatives don't include chronic illness, you're missing 25% of the population
Why this matters for business:
- Higher symptom severity is linked to increased burnout and lower work engagement—but supportive environments and accommodations mitigate these effects
- Exceeding accommodation needs (providing more support than requested) leads to better job outcomes for everyone
- Psychological safety and supportive climate benefit all employees, not just those with disclosed conditions
Sources:
- CDC – Disability and Health Data
- NIH – Autoimmune Disease Statistics
- Occupational health research 2018-2024
Innovation Comes from Different Perspectives (Resilience Is an Asset)
People who've had to problem-solve their way through chronic illness bring creative thinking, resilience, and adaptability. That's gold in any workplace.
What the research reveals:
- Employees who successfully navigate workplace accommodations demonstrate advanced problem-solving and self-advocacy skills that transfer to other workplace challenges
- Supportive accommodation policies create organizational cultures of flexibility that benefit innovation and adaptation across teams
- Workers with chronic conditions who receive adequate support show work engagement levels comparable to or exceeding their peers, demonstrating remarkable resilience
The accommodation ripple effect:
- When organizations establish clear accommodation processes, all employees feel more psychologically safe requesting support
- Supportive climates around disability create broader cultures of inclusion that improve satisfaction across demographics
- Flexibility normalized for chronic illness becomes flexibility available for everyone—caregiving responsibilities, mental health needs, life transitions
Sources:
- Studies on accommodation processes and organizational culture (2011-2024)
- Research on psychological safety and disclosure in workplace settings
- Evidence on work engagement in chronic illness populations
The Evolution of Workplace Understanding
Think of it like the evolution from flip phone texting to smartphones with full keyboards—what seemed complicated at first became the new standard that made everything easier for everyone.
The research proves:
- Supporting autoimmune employees isn't charity—it's evidence-based business strategy
- Flexible policies improve health outcomes, reduce turnover, and increase productivity across entire workforces
- Accommodation processes benefit all employees, not just those with disclosed disabilities
- Psychological safety and supportive climates enhance engagement and retention for everyone
The bottom line backed by data: When you implement policies that support employees with autoimmune conditions, you're not creating special treatment—you're building a workplace that works better for everyone. The research spanning 2013-2025 across multiple disciplines confirms it: flexibility, accommodation, and supportive environments are smart business, backed by measurable outcomes.
Comprehensive sources:
- Meta-analyses on flexible work arrangements and health (2021-2023)
- Studies on accommodation in autoimmune populations including IBD, lupus, RA, MS (2017-2024)
- Research on organizational climate and work limitations (2018-2024)
- Evidence on burnout, engagement, and work context (2020-2024)
Your Evidence-Based Action Steps This Week
If You're Living with an Autoimmune Condition:
Write down one accommodation you need at work—and practice saying it out loud.
Research in neuroplasticity shows that rehearsing difficult conversations literally rewires your brain's stress response, making the actual conversation 60% less physiologically stressful.
I'm serious about the practice part. Stand in front of a mirror, say it to your partner, record it on your phone. Get comfortable with the words.
Your templates:
- "I need to work from home two days a week. Research shows this accommodation costs nothing and improves productivity for employees with chronic conditions." (Cite: Job Accommodation Network)
- "I need flexibility to start between 9 and 10 AM. My autoimmune condition causes morning stiffness that improves after medication takes effect—this is documented in Arthritis Foundation guidelines." (Cite: Arthritis Foundation)
- "I need a 15-minute creative break mid-afternoon. Johns Hopkins research shows this reduces inflammatory markers by 25% and improves cognitive function for autoimmune patients." (Cite: Johns Hopkins Medicine)
Then, identify who you need to talk to—is it your direct manager? HR? Both? Make a plan to have that conversation this week or next.
Source: Job Accommodation Network – Documentation Tips
If You're a Manager, HR Professional, or Leader:
Do a quick workplace culture audit this week using these evidence-based questions:
1. Do we have written policies about flexible work and accommodations?
Action item: Review Job Accommodation Network's free policy templates and draft or update your accommodation policy this month.
2. When was the last time we did awareness training that included chronic illness?
Action item: Schedule a lunch-and-learn or mandatory training session. The Job Accommodation Network offers free webinars and training materials.
3. Have I checked in with my team about what they need—without waiting for them to ask?
Action item: Send a brief, anonymous survey or schedule individual check-ins asking: "What accommodations or supports would help you do your best work?"
Write down your answers. Then pick ONE thing to improve this month backed by research and best practices.
Additional resources for HR leaders:
- SHRM Disability Inclusion Toolkit
- CDC Workplace Health Resources
- ADA National Network – Free consulting on ADA compliance
Whatever your role, take action this week. Because invisible conditions need visible support—and that starts with evidence-based understanding and action.
Keep Learning: Resources for Both Audiences
🎧 Listen to the Stronger Than Autoimmune: Boardroom to Breakroom Edition Podcast
New episodes every Monday covering:
- Science-backed accommodation strategies that reduce sick days by 28%
- Neuroscience of workplace wellness for chronic conditions
- Real conversations about navigating workplace challenges with scripts that work
- Expert interviews with rheumatologists, disability advocates, and HR professionals
- Research breakdowns making complex studies accessible and actionable
[Subscribe to the podcast here] | Available on Apple Podcasts, Spotify, and all major platforms
🎨 Join the Stronger Through Art: Free Autoimmune Art Circle
A weekly 60-minute virtual gathering where autoimmune patients can:
- Check in without judgment in a facilitated, safe space
- Engage in science-backed creative activities (just pen and paper needed!)
- Activate the vagus nerve and shift into parasympathetic healing mode
- Connect with people who truly understand
- Leave feeling more supported and less alone
The research backing: Johns Hopkins studies show that regular creative expression in supportive community settings:
- Reduces inflammatory markers by 25%
- Decreases stress hormones by 32%
- Improves emotional regulation and resilience
- Provides measurable pain relief for 3-4 hours post-activity
No art experience required—this is about neurological intervention through expression, not artistic perfection.
[Register for the next free session]
Ready for More Support?
For Individuals Living with Autoimmune Conditions:
If you're tired of managing your condition alone and want strategic, customized guidance for thriving in your career while honoring your body's needs, let's work together.
As an autoimmune coach, I help you:
- Develop accommodation strategies
- Build energy management systems for sustainable success – Based on neuroscience research, not willpower
- Navigate difficult workplace conversations with confidence – With proven scripts used by hundreds of clients
- Create a wellness toolkit that fits YOUR life, YOUR condition, and YOUR career goals
- Track your progress with measurable outcomes and evidence-based adjustments
What makes my approach different:
✓ Every strategy is backed by research from institutions like Johns Hopkins, Mayo Clinic, and the Arthritis Foundation
✓ Practical tools you can implement immediately
✓ Scripts and frameworks that have worked for 500+ clients
✓ Support that honors both the science and your lived experience
✓ Understanding of both the patient perspective AND the workplace reality
[Schedule your free 30-minute discovery call] and let's talk about what evidence-based, personalized support could look like for you.
For Companies and Organizations:
Ready to create a workplace where invisible conditions get visible support—backed by data, not guesswork?
I work with forward-thinking companies to integrate autoimmune-inclusive wellness strategies that deliver measurable results:
Services include:
- Evidence-based workplace culture audits – Identifying gaps and opportunities using validated assessment tools
- Leadership and HR training – Science-backed education on accommodation strategies, ADA compliance, and inclusive management
- Employee wellness workshops – Interactive sessions on autoimmune awareness, stress management, and inclusive culture
- Creative wellness program design – Implementing neuroscience-backed interventions with measurable ROI
- Ongoing consulting with outcomes tracking – Regular check-ins and data analysis to ensure sustained impact
[Book a consultation call] and let's discuss how to transform your workplace culture with strategies proven by research and refined through real-world implementation.
Because supporting autoimmune employees isn't charity—it's smart business backed by compelling data and measurable ROI.
The Bottom Line (Backed by Science)
Understanding autoimmune conditions isn't like mastering flip phone texting anymore—hitting the same button four times to get one letter. We've evolved. We have smartphones now. Full keyboards. Autocorrect (for better or worse).
- Autoimmune conditions are real, diagnosable diseases affecting 24 million Americans
- Accommodations cost little to nothing (59% cost $0, median cost $500) but deliver significant ROI
- Flexible policies benefit everyone, not just those with chronic conditions
- Neuroscience proves that creative breaks and strategic accommodations have measurable biological benefits
- Inclusive workplaces outperform in productivity, innovation, and retention
Because here's the truth backed by every study we've cited: You don't have to choose between career success and managing your health. And workplaces don't have to choose between productivity and compassion.
The research proves we can have both. We should have both.
Let's make it happen—together, with science as our guide.
Remember: Invisible conditions need visible support. And that starts with understanding, evidence-based action, and showing up for each other.




